The American Academy of Emergency Medicine (AAEM) is highly concerned regarding the recently released Centers for Medicare and Medicaid Services (CMS)’s 2026 Medicare Physician Fee Schedule (PFS) Final Rule, which will reduce the facility practice expense component of Relative Value Units (RVUs) for the most commonly used emergency department visit codes by roughly 20% and for critical care services by 30%.
Facility PE RVUs by Year (ED E/M)
| Code | 2025 | 2026 | % |
| CPT 99281 | 0.06 | 0.05 | -17% |
| CPT 99282 | 0.22 | 0.17 | -23% |
| CPT 99283 | 0.35 | 0.28 | -20% |
| CPT 99284 | 0.57 | 0.45 | -21% |
| CPT 99285 | 0.79 | 0.65 | -18% |
Facility RVUs by Year (Critical Care)
| Code | 2025 | 2026 | % |
| CPT 99291 | 1.42 | 1.00 | -30% |
| CPT 99292 | 0.72 | 0.53 | -26% |
These cuts to the facility practice expense component will reduce the overall value of most emergency department visit codes by roughly 3% and for critical care services by ~7%. These cuts will apply to the over one quarter of all emergency department patients covered by the Medicare program and Tricare program. In addition, many state Medicaid programs tie their reimbursements to the Medicare PFS, as do many private insurer contracts, so these cuts could impact the majority of emergency department patients.
In recent years, emergency physicians have absorbed the smallest increases in compensation of all physician specialties, significantly lagging inflation. Many private insurers have utilized new regulations under the No Surprises Act (NSA) to significantly decrease emergency physician compensation. These 2026 PFS cuts will worsen this trend, leading to significant impacts on emergency medicine. The financial viability of many emergency physician groups will be threatened, which will impact patient access to emergency department care. Emergency physician staffing levels could be negatively affected to maintain emergency physician group solvency, impacting the quality of care.
The majority of emergency physicians are not hospital employees and work in groups that must cover their own practice expenses such as coding/billing, professional liability insurance, and staffing-related services. These costs have not decreased and there is no justification for the 2026 PFS’s dramatic decreases in the practice expense component. AAEM urges CMS to recognize the impact of the 2026 Medicare PFS Final Rule on emergency physician practices and to make appropriate revisions.
Additional Background: Long-Term Medicare Payments Trends
The graph below shows how the conversion factor (CF) used in the Medicare Physician Fee Schedule has generally not kept pace with inflation. This means that the dollar value paid per RVU has been flat or has even dropped at times over the years. Physicians are not immune to the increased cost of living. Additionally, as physician practice expenses, such as supplies and technology, also rise with inflation, a stagnant CF results in a functional decrease in real physician reimbursement. Even when there is a nominal increase in (CF) in a single year, physicians experience a continuous erosion of compensation for the work they perform year after year, making it harder to maintain financial viability.
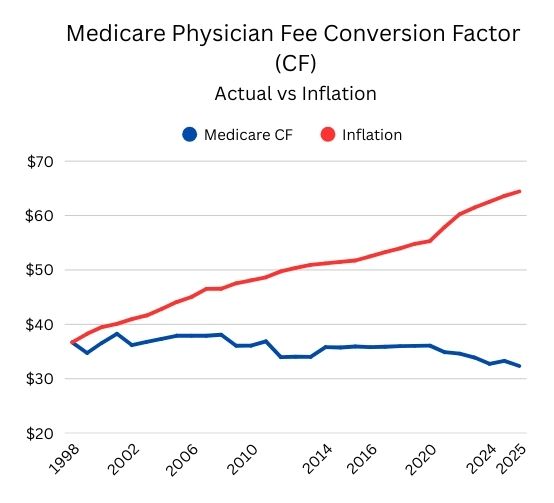
Source: American Medical Association. Data from the Federal Register, Medicare Trustees’ Reports, Bureau of Labor Statistics, and Congressional Budget Office. Updated January 2025.
