April 19-23, 2020 • Sheraton Phoenix Downtown • Phoenix, AZ




Photographs of patients, pathology specimens, Gram stains, EKGs, and radiographic studies or other visual data may be submitted. Photographs of patients and pathology specimens are preferred. Your submission should depict clear examples of findings that are relevant to the practice of emergency medicine or findings of unusual interest that have educational value. If your submission is accepted, you must mount it for viewing.
No more than three different photos may be submitted for any one case.
The Photo Competition is open to all AAEM members and non-members, including residents and students.
Photo submissions must be accompanied by a brief case history and case discussion, written as an “unknown.”
The case history is limited to no more than 250 words and should include:
The case discussion should be brief (ideally no more than 750 words) and must be submitted in a separate MS Word document. The case discussion should include the following information:
Please submit only blind copies, omitting your name, institution, city, state, or any other identifier.
Competitions are now closed.
If accepted for display, AAEM reserves the right to edit the submitted case history. Submissions are selected based on educational merit, relevance to emergency medicine, quality of the photograph, the case history, and appropriateness for public display. If your photograph is accepted, you will be notified and informed of set-up and dismantle times. Patients and patient identifiers must be appropriately masked. Additionally, you must attest that written consent and release of responsibility have been obtained for all photos EXCEPT for isolated diagnostic studies such as EKGs, radiographs, Gram stains, etc.
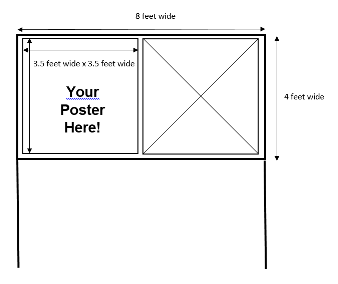
Responsibility for bringing photo and case submission(s) to the Scientific Assembly rests with the submitter. A 3.5´ x 3.5´ square area will be available for each submission.
Notification of Abstract Selection
The presenting author of all abstracts submitted by 11:59pm CST on November 4, 2019, will receive notification of acceptance or rejection in February 2020.
Withdrawals and Revisions
Withdrawals and revisions must be received in writing to Rebecca Sommer at rsommer@aaem.org by November 11, 2019. No changes can be submitted after that date.
Presenting Author Information
Only one individual may submit a photo through the online submission portal. The submitter will serve as the point-of-contact with AAEM. If your submission is accepted for display at Scientific Assembly, you may include the names of co-authors and co-submitters on the display.
Previous Presentations of Photos
Any photo that has been previously published or used in a national conference competition should not be submitted. Photos that have been presented at international meetings (MEMC) and have not been published, can be submitted for consideration.
Funding
Indicate what monies have funded the research.
Disclosure of Relevant Financial Relationships
In accordance with the essentials and standards set forth by the Accreditation Council for Continuing Medical Education, as well as guidelines proposed by the Food and Drug Administration and endorsed by the American Medical Association, an author with a conflict of interest with the content of their abstract must disclose that conflict prior to presentation. A conflict of interest includes, but is not limited to, any relevant financial relationship in a company, product or procedure mentioned in the abstract or in the presentation to be given at the conference. The authors must complete the disclosure form included in the electronic submission. A conflict in and of itself will not eliminate an abstract from consideration.
Informed Consent
Any studies involving human subjects must conform to the principles of the Declaration of Helsinki of the World Medical Association (Clinical Research 1966; 14:103) and must meet all the requirements governing informed consent of the country in which the research was performed.
Abstract Publication
Posters presented at AAEM’s 26th Annual Scientific Assembly may be published on the AAEM website and shared via social media.
Use of Cases for Education
Submitters will be asked for permission for AAEM to use accepted cases for online continuing medical education purposes. All authors and contributors will be appropriately credited.
The photo competition continues to be a highlight at our annual convention--both unique and thought provoking, it serves as opportunity to share visual patient encounters to enhance the practice of any practioner, young or seasoned. Last year's winner is no exception...highlighting an interesting eye case that is both thought provoking and has many well outlined teachable points. We look forward to again showcasing the 2020 winning case!
— Bob Zemple, MD FAAEM
Chief complaint: Left eye injury
History of present illness: 21-year-old female presents with a left eye injury that occurred the day prior. Patient states she was rushing and was putting her jacket on when the zipper struck her in the left eye. Patient states she woke up in the morning and found her left eye appeared odd, with a cloudy spot and a bulging appearance. Patient denies pain, vision changes, photo sensitivity, eye discharge or tearing. Patient states she wears glasses regularly but denies contact use.
Pertinent physical exam: Eye exam: EOMI, PERRLA, no pain on extraocular movements. There is a focal opaque area of stoma corneal edema that is markedly elevated compared to the rest of the corneal. No epithelium defect noted. Vision testing: 20/200 left eye and 20/70 on the right, without glasses. Fluorescein stain: mild uptake at the 3 o’clock position. No hyphema was noted. A slit lamp examination demonstrated a conical protrusion from the cornea not in the visual field. Negative Seidel sign.
Questions



Answers:
Case Discussion:
Patient was evaluated at bedside by the ED resident and attending. Visually notable defect on the anterior surface of the left eye was examined. Fluorescein stain did show mild uptake at 3 o’clock position. Visual acuity exam was performed and was at baseline for the patient.
Ophthalmology was consulted, and the case was discussed. Since the patient was comfortable at bedside with no complaints of pain, visual acuity change, and no Seidel sign noted, it was decided that no emergent interventions were needed. The patient was discharged with ophthalmology follow-up the next morning and given a prescription for ciprofloxacin eyedrops.
Upon further questioning, patient stated that she had corrective glasses since she was a child but never had perfect vision. Patient stated she consistently has changing prescriptions for her glasses. Follow up with patient and ophthalmologist was done and patient was diagnosed with corneal hydrops from an undiagnosed keratoconus. Patient was given a course of hypertonic saline eye drops and referral to an anterior chamber specialist for contact lens fitting.
Pearls: